Convenience has become a top priority in the digital age for all service sectors, including healthcare. Telemedicine has been a game-changer in contemporary healthcare as the globe continues to move towards digital-first solutions. Telemedicine app development is now a strategic necessity for entrepreneurs and healthcare providers, as the worldwide telemedicine app development market is expected to reach $286 billion by 2030.
This blog serves as a comprehensive guide to telemedicine app development, covering every critical element from planning and features to compliance and monetization strategies.
Types of Telemedicine Apps
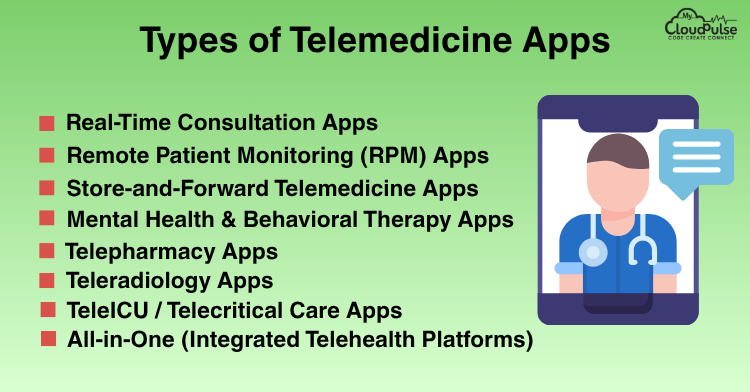
Telemedicine is not a one-size-fits-all solution. Depending on the healthcare need, there are various types of telemedicine apps, each designed to solve specific problems for patients and healthcare providers. Choosing the right type (or a hybrid model) is critical to aligning with your goals.
Real-Time Consultation Apps
Description:
These apps allow patients and healthcare providers to connect via live video, audio, or chat for instant diagnosis and treatment.
Key Features:
- Video/audio call integration
- Real-time chat support
- Appointment booking & calendar sync
- E-prescriptions
- Doctor notes & follow-up reminders
Ideal For:
- General practitioners, specialists
- Emergency consultations
- Rural/remote patients
- Mental health and therapy services
Benefits:
- Immediate access to healthcare
- Reduces wait time and travel
- Convenient for minor and moderate health issues
Remote Patient Monitoring (RPM) Apps
Description:
These apps help monitor patients’ chronic conditions or post-surgery recovery using connected medical devices and wearables that transmit data to doctors in real time.
Key Features:
- IoT device integration (BP monitors, glucose meters, etc.)
- Real-time vitals tracking
- Alerts for abnormal health readings
- Data visualization (charts/graphs)
- Doctor dashboards for ongoing monitoring
Ideal For:
- Chronic disease management (diabetes, heart disease, COPD)
- Elderly care
- Post-operative recovery
- Hospitals and home healthcare providers
Benefits:
- Early detection of health risks
- Reduces hospital readmissions
- Enables continuous care without in-person visits
Store-and-Forward Telemedicine Apps (Asynchronous Care)
Description:
Patients can upload their symptoms, medical images, and lab reports, which doctors review and respond to later — no live interaction required.
Key Features:
- File upload (X-rays, lab results, photos)
- Asynchronous messaging
- Doctor review queue
- Notification of doctor response
- Prescription and advice delivery
Ideal For:
- Dermatology, radiology, pathology
- Non-urgent consultations
- Rural clinics with bandwidth limitations
Benefits:
- Saves time for both doctors and patients
- Useful in areas with limited internet or time zones
- Improves access to specialist care
Mental Health & Behavioral Therapy Apps
Description:
These apps are tailored for online therapy, counseling, and mental wellness, providing access to licensed psychologists, therapists, or AI-guided self-care tools.
Key Features:
- Anonymous therapy sessions
- One-on-one video counseling
- Mood tracking & journaling
- AI chatbots for CBT (Cognitive Behavioral Therapy)
- Meditation and breathing exercises
Ideal For:
- Individuals facing anxiety, stress, depression
- Corporate wellness programs
- College/university student support
- Teen and youth mental health services
Benefits:
- Breaks stigma by offering privacy
- Available anytime, anywhere
- Encourages consistency in mental health care
Telepharmacy Apps
Description:
These apps provide online pharmacy services, letting patients receive e-prescriptions, order medicines, and have them delivered to their homes.
Key Features:
- Prescription upload & verification
- Doctor/pharmacist consultation
- Medicine catalog with search
- Refill alerts and subscriptions
- Order tracking and payment gateway
Ideal For:
- Patients needing regular medications
- People with limited mobility or in rural areas
- Clinics offering bundled care + pharmacy delivery
Benefits:
- Streamlines the treatment lifecycle
- Saves patients time and effort
- Reduces prescription errors through automation
Teleradiology Apps
Description:
Specifically designed for radiologists to receive, view, and interpret medical images (X-rays, CT scans, MRIs) remotely.
Key Features:
- High-resolution DICOM image viewer
- Annotation tools
- Reporting templates
- PACS integration
- Secure image sharing with hospitals
Ideal for:
- Hospitals with limited radiology staff
- Emergency trauma units
- Multi-location diagnostic labs
Benefits:
- Enables 24/7 radiology reporting
- Supports faster diagnosis in emergencies
- Reduces costs for healthcare providers
TeleICU / Telecritical Care Apps
Description:
Used in Intensive Care Units (ICUs) where remote critical care specialists monitor patient vitals and guide on-ground staff.
Key Features:
- Real-time patient monitoring
- Vital tracking dashboards
- Video/audio conference with ICU teams
- Alerts for intervention
- Centralized specialist access
Ideal For:
- Hospitals in tier-2/tier-3 cities
- Facilities with high patient load and fewer specialists
- Emergency response teams
Benefits:
- Improves outcomes in critical situations
- Gives remote hospitals access to specialized care
- Reduces ICU mortality rates
All-in-One (Integrated Telehealth Platforms)
Description:
These are comprehensive platforms that combine multiple services like consultation, diagnostics, pharmacy, and wellness into a single app.
Key Features:
Real-time and asynchronous consultations
- Lab test bookings
- Medicine delivery
- EHR management
- Health insurance integration
- AI-based triage and recommendations
Ideal For:
- Large hospitals and healthcare networks
- Insurance companies
- Government health programs
Benefits:
- One-stop solution for users
- Streamlines operations and user engagement
- Ideal for scaling and cross-selling services
Challenges in Telemedicine App Development
While telemedicine offers significant advantages — like remote access to care, cost-efficiency, and convenience — building and operating a telemedicine app comes with its own set of complex challenges. These challenges span across technical, regulatory, clinical, and user experience dimensions.
Data Privacy & Security Concerns
The Challenge:
Handling sensitive personal health information (PHI) digitally makes telemedicine apps highly vulnerable to cyberattacks, data breaches, and identity theft.
Why it Matters:
Healthcare data is one of the most targeted and valuable assets for hackers. Non-compliance with standards like HIPAA, GDPR, or NDHM can result in heavy fines and legal consequences.
Solution:
- End-to-end encryption (for data in transit and at rest)
- Two-factor authentication (2FA)
- Regular vulnerability scans and audits
- Role-based access control and tokenized sessions
Maintaining High-Quality Video & Audio Communication
The Challenge:
Poor network connectivity, low-resolution video, or lags can hinder accurate diagnosis, especially in remote or rural areas with unstable internet.
Why it Matters:
Real-time interaction is crucial for building patient trust and enabling doctors to visually assess symptoms (e.g., rashes, swelling, etc.).
Solution:
- Use of adaptive bitrate streaming with APIs like WebRTC, Agora, or Twilio
- Support for low-bandwidth environments
- Allow fallback to voice or chat mode
Licensing & Cross-Border Regulatory Issues
The Challenge:
Doctors often face legal limitations in treating patients outside their licensed state or country. Additionally, healthcare regulations vary significantly across regions.
Why it Matters:
This hinders telemedicine expansion and can result in illegal practice accusations if not properly managed.
Solution:
- Geo-restricted doctor-patient pairing
- Maintain dynamic legal compliance modules
- Partner with legal advisors or local regulatory consultants
Lack of Physical Examination
The Challenge:
Without the ability to touch, palpate, or run physical diagnostics, physicians may find it difficult to provide comprehensive care in some situations.
Why it Matters:
This limitation can lead to misdiagnosis or underdiagnosis in cases where physical signs are essential (e.g., orthopedics, cardiology).
Solution:
- Integrate AI-assisted symptom checkers
- Use remote diagnostic devices (e.g., pulse oximeters, glucose meters, wearables)
- Enable hybrid models — virtual first, in-person follow-up when needed
Low Digital Literacy Among Patients
The Challenge:
Some patients — particularly the elderly or those in rural regions — may struggle with using mobile apps, video calls, or digital prescriptions.
Why it Matters:
This can result in lower app adoption, user frustration, or even medical errors.
Solution:
- Provide multilingual, voice-guided interfaces
- Design ultra-simplified UI/UX
- Offer assisted teleconsultation via healthcare staff or call centers
Doctor & Patient Adoption Resistance
The Challenge:
Many doctors may be hesitant to shift from traditional in-clinic models to digital platforms, fearing income loss, tech burden, or legal complexities. Similarly, patients may distrust virtual care quality.
Why it Matters:
Adoption by both users is crucial for telemedicine success. Without their trust, even the best tech fails.
Solution:
- Offer onboarding sessions and training
- Highlight convenience, income potential, and safety
- Ensure legal clarity and malpractice protection for doctors
Scheduling Conflicts and Time Zone Barriers
The Challenge:
Managing appointments, cancellations, and time zone differences — especially in international platforms — can become complex.
Why it Matters:
Missed appointments or scheduling errors impact patient satisfaction and revenue.
Solution:
- Implement auto-time zone adjustment
- Real-time calendar sync with buffer periods
- Instant rescheduling and notifications
Integration with Existing Healthcare Systems (EHR/EMR)
The Challenge:
Seamlessly connecting your telemedicine platform with hospital systems, labs, pharmacies, and insurance databases is often difficult.
Why it Matters:
Lack of integration creates workflow silos, repeated data entry, and medical errors.
Solution:
- Use industry-standard protocols like FHIR or HL7
- Provide secure APIs for third-party systems
- Offer modular integration options during onboarding
Reimbursement & Insurance Complications
The Challenge:
Telemedicine services are not always reimbursed at the same rate as in-person care, and insurance rules vary by region and provider.
Why it Matters:
This affects affordability for patients and sustainability for doctors or clinics.
Solution:
- Partner with insurers or digital health plans
- Integrate insurance claim APIs
- Clearly show consultation costs and coverage eligibility before booking
Ensuring Clinical Accuracy & Standardization
The Challenge:
There’s often a lack of standard guidelines for clinical decision-making in telemedicine, which can affect care quality.
Why it Matters:
Standardization ensures that telemedicine consultations match (or exceed) the quality of physical visits.
Solution:
- Use clinical decision support systems (CDSS)
- Follow evidence-based care protocols
- Include specialist referrals for complex cases
Future Trends in Telemedicine App Development (2025 & Beyond)
As telemedicine matures from a pandemic-driven necessity to a core pillar of modern healthcare, the industry is now witnessing a wave of innovation. Emerging technologies such as AI, IoT, AR/VR, and Blockchain are transforming how virtual care is delivered — making it smarter, more personalized, and more scalable.
Below are the top telemedicine trends that will define the future of digital healthcare.
AI-Powered Triage & Virtual Assistants
What’s Happening:
AI chatbots and symptom checkers are becoming the first point of contact in many telemedicine platforms. These tools collect patient information, assess symptoms, and direct users to the appropriate care level.
Use Cases:
- Pre-consultation symptom assessment
- Scheduling the right type of doctor
- Answering FAQs and guiding users through the app
Impact:
- Reduces workload on doctors
- Speeds up the care delivery process
- Improves triage accuracy and patient satisfaction
Integration with Wearables & IoT Devices
What’s Happening:
Smart health wearables like Apple Watch, Fitbit, and glucose monitors are now being integrated directly into telemedicine apps. These devices send real-time health data to doctors for better decision-making.
Use Cases:
- Remote monitoring of vitals (heart rate, blood pressure, oxygen levels)
- Chronic disease management (e.g., diabetes, hypertension)
- Post-operative care and elderly support
Impact:
- Enables proactive healthcare instead of reactive treatment
- Enhances accuracy of virtual diagnosis
- Allows for 24/7 patient tracking and alerts
Voice-Enabled Interfaces & Voice-to-Text Features
What’s Happening:
Voice technology is improving accessibility and convenience for users, especially in rural areas or among elderly patients.
Use Cases:
- Voice-based symptom reporting
- Doctors dictating prescriptions or notes using voice
- Hands-free app navigation for users with disabilities
Impact:
- Makes apps more inclusive and user-friendly
- Saves doctors time during consultations
- Reduces the need for typing or form-filling
AR/VR for Enhanced Remote Diagnosis & Therapy
What’s Happening:
Augmented Reality (AR) and Virtual Reality (VR) are being explored for use in remote diagnosis, physical therapy, and even mental health therapy.
Use Cases:
- Simulated therapy environments for PTSD, anxiety, and phobias
- Remote physical rehabilitation with visual aids and posture tracking
- AR tools for guiding patients through self-examinations
Impact:
- Improves the quality of remote assessments
- Engages patients more effectively in therapy
- Reduces the need for in-person visits in specific fields
Blockchain for Secure Health Data Sharing
What’s Happening:
Blockchain technology offers a decentralized and secure method for storing and sharing patient health records without compromising privacy.
Use Cases:
- Health data exchange between clinics, labs, and insurers
- Secure patient ID management
- Consent management and access tracking
Impact:
- Enhances data transparency and trust
- Prevents fraud or tampering of medical records
- Gives patients more control over their health information
Predictive Analytics & Personalized Healthcare
What’s Happening:
With access to large volumes of patient data, AI can now analyze trends and predict future health outcomes or risks.
Use Cases:
- Predicting likelihood of disease progression
- Personalized treatment suggestions
- Risk alerts for chronic patients
Impact:
- Improves preventive care
- Increases efficiency in treatment planning
- Offers hyper-personalized patient experiences
Multilingual and Regional Language Support
What’s Happening:
With telemedicine becoming more global, platforms are incorporating multilingual interfaces and AI-powered translation tools to bridge communication gaps.
Use Cases:
- Real-time speech translation during doctor-patient video calls
- Multilingual content and chatbots
- Regional voice assistants for rural areas
Impact:
- Expands telemedicine reach to underserved populations
- Reduces language barriers in healthcare delivery
- Improves trust and clarity in doctor-patient communication
Hybrid Healthcare Models (Click-and-Mortar)
What’s Happening:
The future is not entirely virtual. Many providers are now adopting hybrid models, offering both telemedicine and physical visits — depending on the case severity.
Use Cases:
- Initial consultations online, physical exams offline
- Automated routing from virtual to in-person when necessary
- In-clinic follow-ups for complex treatments
Impact:
- Increases flexibility in care delivery
- Provides comprehensive patient coverage
- Enhances doctor-patient relationships
Telemedicine App Development in Specialized Fields
What’s Happening:
Telemedicine is now expanding beyond general medicine to fields like dermatology, ophthalmology, psychiatry, pediatrics, and even oncology.
Use Cases:
- Skin condition diagnosis through image upload (teledermatology)
- Virtual eye tests and vision therapy
- Pediatric care and parental guidance sessions
Impact:
- Unlocks virtual care potential in specialist domains
- Reduces wait times and costs for specialty consultations
- Encourages early diagnosis and intervention
Interoperability & EHR Integration
What’s Happening:
Future-ready telemedicine apps are being built with interoperability in mind — the ability to seamlessly share data across platforms and systems.
Use Cases:
- Syncing patient records from clinics, hospitals, labs, and insurers
- Faster referral process between doctors and departments
- Unified patient health records accessible across providers
Impact:
- Prevents duplication of care or diagnostics
- Ensures continuity in patient treatment
- Improves accuracy and safety of care
Final Thoughts
Choosing the right type of telemedicine app development depends on your specific goals, users, budget, and the healthcare services you plan to offer. You can start small say, with a live consultation app and later integrate other modules like pharmacy or remote monitoring as your platform evolves.
Whether you’re a hospital, clinic, startup, or healthtech entrepreneur, understanding these app types will help you prioritize features, choose the right tech stack, and create a better user experience.